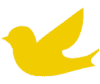
What Is the Microbiome?
The scientific literature claims that the human microbiome should be considered an organ or even a “super-organism.” Discovered as recently as the 1990s, the microbiome is now known to have a powerful impact on our human health. The term “microbiome” is referred to by experts as the collection of the genomes of microbes in a particular ecosystem. The term “microbiota” is referred to as the collection of organisms.
The entire digestive tract is a living ecological community of microorganisms – over 100 trillion bacteria – which we call the microbiome. What is even more astonishing is that over 70% of our immune system is influenced and shaped by the enteric bacteria or gut flora found in the microbiome of the gastrointestinal tract. There is an intrinsic, complex interaction among the gut, the immune system, and even the nervous system, which includes our brains!
Gut-Brain-Immune System
You might have heard the terms “gut-brain-connection”, “the second brain”, or the “gut-brain-axis“. These all refer to the communication between the central and enteric (gut) nervous system – the connection between the emotional and cognitive centers of the brain and the gastrointestinal system. The gut and brain communicate bi-directionally, AND they also communicate with the immune system. Neurons and their chemical messengers called neurotransmitters are found in the brain and they also exist in the gut, or enteric nervous system, a vast mesh like matrix of nerves housed in the intestines. Half of the body’s dopamine and 95% percent of the body’s serotonin are actually produced in the gut!
The gut and the brain both rely on an autonomic (or automatic) nervous system (ANS). The system that governs the gut is usually referred to as the enteric nervous system (ENS). When the ANS is operating normally and senses danger or stress, it activates a sympathetic state that we often call “fight-flight-or-freeze.” When there is no, or low, stress in a body, it can enter the parasympathetic, or “rest-and-digest” state. Our immune system must keep in step with the demands of the changing landscape of stress and safety in our bodies too. Along with the nervous system, the immune system runs surveillance to protect us from harm while allowing our bodies to continue to function, grow, repair, and ultimately thrive.
Because of the intimate, co-dependent relationship between the gut inhabitants (a so-called super organism) and other body systems, when there are alterations in the make-up or functioning of the microbiome, there are not merely intestinal consequences. Changes in the microbiome also impact our brains and immune system. Scientific research is repeatedly showing us that LOW bacterial diversity in the gut is associated with worse health outcomes (see Sources & References, below). Nowhere is this more obvious than in children with autism spectrum disorders who express behavioral abnormalities, cognitive deficits, developmental delays, sensory issues, immune dysregulation, typically have signs or symptoms of poor gut health AND poor microbiome diversity.
What’s in the Gut – a Diverse Microbiome or Dysbiosis?
Derrick MacFabe MD, PhD, a Canadian researcher, was actually the first researcher to scientifically prove this gut-brain-immune connection through mouse studies. He discovered how gut bacteria can alter behaviors in children with autism. Dr. MacFabe found that children with autism had a history of antibiotic exposure or hospitalization, gastrointestinal symptoms, abnormal food cravings and unique intestinal bacterial populations that were related to the severity of their symptoms.
His research on the role of enteric short-chain fatty acid fermentation products, in particular one strain called proprionic acid (PPA), a toxic metabolite of Clostridia difficile (C. diff), was found in the gastrointestinal tract of children with autism. PPA is a compound of many gastrointestinal bacteria and a common food preservative. It and other metabolites of gut pathogens (colletively known as gut dysbiosis) can cause neurochemical changes that are all consistent with autism findings, such as:
- Neuroinflammation
- Oxidative stress
- Mitochondrial dysfunction
- Glutathione depletion
- Altered phospholipid/acetylcarnitine levels
The results from laboratory studies showed that rats treated with PPA developed behaviors similar to autism such as repetitive, perseverative, antisocial behaviors and seizures. Metabolites (or substances formed by) gut pathogens affect many important aspects of our bodies such as”
- Neurotransmitters
- Intracellular acidification
- Calcium release
- Fatty acid metabolism
- Immune function
- Alteration of gene expression
Environmental triggers may be part of gut dysbiosis, and it is quite clear that the role of the microbiome has an effect on metabolism, immune, mitochondrial function and gene expression in children with autism as well as those with other chronic health conditions.
Healing the Microbiome
Healing the microbiome can make many positive changes in your child, such as:
- Reducing histamine and inflammation responses
- Reducing the intensity of anxiety and depression (anger in many cases)
- Reducing the self-stimulatory behaviors
- Reducing head-banging and self-mutilating behaviors
- Reducing hand-flapping
- Reducing pacing and hyperactivity
- Reducing the number of meltdowns
- Reducing repetitive and obsessive compulsive behaviors
- Improving sleep issues
- Improving coping abilities
- Strengthening and improving the immune system
- Improving sensory processing
Better Diet for a Better Microbiome
Diet plays a big role in the elimination of gut pathogens (the harmful organisms) in the gastrointestinal tract. A typical modern-day acidic diet of refined sugars, high fructose, simple carbohydrates, gluten, casein, trans-fatty acids, fast foods with chemical preservatives, and refined foods increase gut dysbiosis in the digestive tract and affect the brain and the immune system.
If your child is eating a high carbohydrate and rich food diet, then the likelihood of gut dysbiosis is much higher. Gut dysbiosis increases acidity and can create more physical symptoms as well as behaviors. To lower levels of gut pathogens, give your child a diet rich in:
- Fermented foods and vegetables
- Kefir non-dairy yogurt
- Organic vegetables, fruits and protein
- Good quality fats
- Lots of prebiotics and probiotics
- A gut-healing diet
These will typically help heal the microbiome by alkalizing the gut and creating more butyrate in the gut which is necessary for restoring gut integrity. Other supports can be put into place to heal a gut that lacks integrity, too. Rebalancing the gut microbiota by healing the microbiome will improve the gut lining and brain function, reduce behaviors, and keep the immune system stronger.
A practitioner who is “gut literate” may want to help you lower certain pathogens before embarking on certain enriching foods. For instance, if yeast is something that is overgrown in the gut, you may want to start with healthy fats and fiber rich foods or use herbs before introducing fermented foods. To test for imbalances in the microbiome, your provider may want to order an Organic Acid Test (OAT) and/or a Comprehensive Digestive Stool Analysis.
Still Looking for Answers?
Visit the Documenting Hope Practitioner Directory to find a practitioner near you.
Join us inside our online membership community for parents, Healing Together, where you’ll find even more healing resources, expert guidance, and a community to support you every step of your child’s healing journey.
Sources & References
Adams, J.B., et al. Gastrointestinal Flora and Gastrointestinal Status in Children with Autism—Comparisons to Typical Children and Correlation with Autism Severity. BMC Gastroenterol. 2011;11:22.
Aguilera, M., et al. Antibiotic-induced dysbiosis alters host-bacterial interactions and leads to colonic sensory and motor changes in mice. Gut Microbes. 2015;6(1):10-23.
Appleton, J. The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health. Integr Med (Encinitas). 2018 Aug;17(4):28-32.
Aroniadis, O.C., et al. Fecal microbiota transplantation: past, present and future. Curr Opin Gastroenterol. 2013;29(1):79-84.
Assa, A., et al. Vitamin D deficiency promotes epithelial barrier dysfunction and intestinal inflammation. J Infect Dis. 2014;210(8):1296-305.
Atladóttir, H.Ó., et al. Autism after infection, febrile episodes, and antibiotic use during pregnancy: an exploratory study. Pediatrics. 2012 Dec;130(6):e1447-54.
Aversa, Z., et al. Association of Infant Antibiotic Exposure With Childhood Health Outcomes. Mayo Clin Proc. 2020 Nov 6;S0025-6196(20)30785-0.
Bäckhed, F., et al. Host-Bacterial Mutualism in the Human Intestine. Science. 2005 Mar 25;307(5717):1915-20.
Bennings, M.A., et al. Colonic transit times and behaviour profiles in children with defecation disorders. Archives of the Diseases of Childhood. 2004 Jan;89(1):13-6.
Berding, K., et al. Diet Can Impact Microbiota Composition in Children With Autism Spectrum Disorder. Front. Neurosci. 2018;12:515.
Bjørklund, G., et al. Gastrointestinal alterations in autism spectrum disorder: What do we know? Neurosci Biobehav Rev. 2020 Nov:118:111-120.
Bora, S.A., et al. Regulation of vitamin D metabolism following disruption of the microbiota using broad spectrum antibiotics. J Nutr Biochem. 2018 Jun;56:65-73.
Borchers, A.T., et al. Probiotics and immunity. Journal of Gastroenterology. 44 (2009): 26-46.
Borre, Y.E., et al. Microbiota and neurodevelopmental windows: implications for brain disorders. Trends Mol Med. 2014 Sep;20(9):509-18.
Bruzzese, E., et al. Disrupted intestinal microbiota and intestinal inflammation in children with cystic fibrosis and its restoration with Lactobacillus GG: a randomised clinical trial. PLoS One. 2014 Feb 19;9(2):e87796.
Buccigrossi, V., et al. Functions of intestinal microflora in children. Curr Opin Gastroenterol. 2013;29(1):31-8.
Buie, T., et al. Evaluation, diagnosis, and treatment of gastrointestinal disorders in individuals with ASDs: a consensus report. Pediatrics. 2010 Jan;125 Suppl 1:S1-18.
Camilleri, M. Serotonin in the gastrointestinal tract. Curr Opin Endrocrinol Diabetes Obes. 2009 Feb;16(1):53-9.
Carding, S., et al. Dysbiosis of the gut microbiota in disease. Microb Ecol Health Dis. 2015;26:26191.
Chen, C.Q., et al. Distribution, function and physiological role of melatonin in the lower gut. World J Gastroenterol. 2011 Sep 14;17(34):3888-98.
Chen, Y., et al. Regulation of Neurotransmitters by the Gut Microbiota and Effects on Cognition in Neurological Disorders. Nutrients. 2021 Jun 19;13(6):2099.
Clark, J.A., et al. Intestinal crosstalk—a new paradigm for understanding the gut as the ‘motor’ of critical illness. Shock. 2007 Oct;28(4):384-93.
Cohen-Mekelburg, S., et al. Morning light treatment for inflammatory bowel disease: a clinical trial. BMC Gastroenterol. 2024 May 22;24(1):179.
Correale, J., et al. The role of the gut microbiota in multiple sclerosis. Nat Rev Neurol. 2022 Sep;18(9):544-558.
Critchfield, et al. The potential role of probiotics in the management of childhood autism spectrum disorders. Gastroenterol Res Pract. 2011;2011:161358.
Cucchiara, S., et al. Interactions between intestinal microbiota and innate immune system in pediatric inflammatory bowel disease. J Clin Gastroenterol. 2012;46 Suppl:S64-6.
Cui, J., et al. Butyrate-Producing Bacteria and Insulin Homeostasis: The Microbiome and Insulin Longitudinal Evaluation Study (MILES). Diabetes. 2022 Nov 1;71(11):2438-2446.
da Costa Baptista, I.P., et al. Effect of the use of probiotics in the treatment of children with atopic dermatitis; a literature review. Nutr Hosp. 2013 Jan-Feb;28(1):16-26.
de Goffau, et al. Fecal microbiota composition differs between children with beta-cell autoimmunity and those without. Diabetes. 2013;62(4):1238-44.
D’Eufemia, P., et al. Abnormal intestinal permeability in children with autism. Acta Paediatr. 1996 Sep;85(9):1076-9.
de Magistris, et al. Alterations of the intestinal barrier in patients with autism spectrum disorders and in their first-degree relatives. J Pediatr Gastroenterol Nutr. 2010;51(4):418-24.
Derrien, M., et al. The Gut Microbiota in the First Decade of Life. Trends Microbiol. 2019 Dec;27(12):997-1010.
Dinan, T.G., et al. The Microbiome-Gut-Brain Axis in Health and Disease. Gastroenterol Clin North Am. 2017 Mar;46(1):77-89.
Drago, L., et al. Changing of fecal flora and clinical effect of L. salivarius LS01 in adults with atopic dermatitis. J Clin Gastroenterol. 2012 Oct:46 Suppl:S56-63.
Dogra, S.K., et al. Gut Microbiota Resilience: Definition, Link to Health and Strategies for Intervention. Front Microbiol. 2020 Sep 15:11:572921.
Edwards, C.A., et al. Intestinal flora during the first months of life: new perspectives. British Journal of Nutrition. 88 (2002): S11-S18.
Erickson, C.A., et al. Gastrointestinal Factors in Autistic Disorder: A Critical Review. Journal of Autism and Developmental Disorders. 2005 Dec;35(6):713-27.
Etxeberria, U., et al. Reshaping faecal gut microbiota composition by the intake of trans-resveratrol and quercetin in high-fat sucrose diet-fed rats. J Nutr Biochem. 2015 Jun;26(6):651-60.
Fattorusso, A., et al. Autism Spectrum Disorders and the Gut Microbiota. Nutrients. 2019 Feb 28;11(3):521.
Feng, P., et al. A review of probiotics in the treatment of autism spectrum disorders: Perspectives from the gut-brain axis. Front Microbiol. 2023 Mar 16:14:1123462.
Fukuda, K., et al. Determination of the discriminant score of intestinal microbiota as a biomarker of disease activity in patients with ulcerative colitis. BMC Gastroenterol. 2014;14:49.
Galland, L. The gut microbiome and the brain. J Med Food 2014; 17(12): 1261-72.
Ganal-Vonarburg, S.C., et al. Microbial-host molecular exchange and its functional consequences in early mammalian life. Science. 2020 May 8;368(6491):604-607.
Gastrointestinal permeability in food-allergic children. Nutr Rev. 1985 Aug;43(8):233-5.
Grizotte-Lake, M., et al. Commensals Suppress Intestinal Epithelial Cell Retinoic Acid Synthesis to Regulate Interleukin-22 Activity and Prevent Microbial Dysbiosis. Immunity. 2018 Dec 18;49(6):1103-1115.e6.
Guandalini, S. Are probiotics or prebiotics useful in pediatric irritable bowel syndrome or inflammatory bowel disease? Front Med (Lausanne). 2014;1:23.
Guandalini, S., et al. Prebiotics and probiotics in irritable bowel syndrome and inflammatory bowel disease in children. Benef Microbes. 2015;6(2):209-17.
Hamad, A.F., et al. Prenatal antibiotics exposure and the risk of autism spectrum disorders: A population-based cohort study. PLoS One. 2019 Aug 29;14(8):e0221921.
Han, H., et al. Gut Microbiota and Type 1 Diabetes. Int J Mol Sci. 2018 Mar 27;19(4):995.
Hanaway, P. Balance of Flora, GALT, and Mucosal Integrity. Alternative Therapies in Health and Medicine. Sep-Oct 2006;12(5):52-60; quiz 61-2.
Hejitz, R.D., et al. Normal gut microbiota modulates brain development and behavior. Proc Natl Acad Sci U S A. 2011 Feb 15;108(7):3047-52.
Horn, J., et al. Role of Diet and Its Effects on the Gut Microbiome in the Pathophysiology of Mental Disorders. Transl. Psychiatry. 2022;12:164.
Horvath, K., et al. Autism and gastrointestinal symptoms. Curr Gastroenterol Rep. 2002 Jun;4(3):251-8.
Horvath, K., et al. Autistic disorder and gastrointestinal disease. Current Opinion in Pediatrics. 2002 Oct;14(5):583-7.
Horvath, K., et al. Gastrointestinal abnormalities in children with autistic disorder. Journal of Pediatrics. 1999 Nov;135(5):559-63.
Hrncir, T., et al. Gut microbiota and lipopolysaccharide content of the diet influence development of regulatory T cells: studies in germ-free mice. BMC Immunology. 9 (2008): 65.
Hyman, M.A. Is the Cure for Brain Disorders Outside the Brain? Alternative Therapies in Health and Medicine. Nov-Dec 2007;13(6):10-5.
Isaksson, J., et al. Brief Report: Association Between Autism Spectrum Disorder, Gastrointestinal Problems and Perinatal Risk Factors Within Sibling Pairs. J Autism Dev Disord. 2017 Aug;47(8):2621-2627.
Jackson, P.G., et al. Intestinal permeability in patients with eczema and food allergy. Lancet. 1981 Jun 13;1(8233):1285-6.
Jakobsen, C., et al. Environmental factors and risk of developing paediatric inflammatory bowel disease — a population based study. 2007-2009. J Crohns Colitis. 2013;7(1):79-88.
Jyonouchi, H., et al. Dysregulated innate immune responses in young children with autism spectrum disorders: their relationship to gastrointestinal symptoms and dietary intervention. Neuropsychobiology. 2005;51(2):77-85.
Jyonouchi, H., et al. Evaluation of an Association between Gastrointestinal Symptoms and Cytokine Production against Common Dietary Proteins in Children with Autism Spectrum Disorders. J. Pediatr. 2005;146:605–610.
Kang, D.W., et al. Long-term benefit of Microbiota Transfer Therapy on autism symptoms and gut microbiota. Scientific Reports. 9, 5821 (2019).
Kang, D.W., et al. Microbiota Transfer Therapy alters gut ecosystem and improves gastrointestinal and autism symptoms: an open-label study. Microbiome.2017 Jan 23;5(1):10.
Karagözlü, S., et al. The Relationship of Severity of Autism with Gastrointestinal Symptoms and Serum Zonulin Levels in Autistic Children. J. Autism Dev. Disord. 2022;52:623–629.
Kelly, J.R., et al. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci. 2015 Oct 14;9:392.
Kim-Lee, C., et al. Gastrointestinal disease in Sjogren's syndrome: related to food hypersensitivities. Springerplus. 2015 Dec 12;4:766.
Kitano, H., et al. Robustness trade-offs and host-microbial symbiosis in the immune system. Molecular Systems Biology. 2 (2006).
Kobliner, V., et al. Reduction in Obsessive Compulsive Disorder and Self-Injurious Behavior With Saccharomyces boulardii in a Child with Autism: A Case Report. Integr Med (Encinitas). 2018 Dec;17(6):38-41.
Korpela, K., et al. Maternal Fecal Microbiota Transplantation in Cesarean-Born Infants Rapidly Restores Normal Gut Microbial Development: A Proof-of-Concept Study. Cell, 2020.
Lai, C.C.W., et al. The association between gut-health promoting diet and depression: A mediation analysis. J Affect Disord. 2023 Mar 1:324:136-142.
Lavebratt, C., et al. Early exposure to antibiotic drugs and risk for psychiatric disorders: a population-based study. Transl Psychiatry. 2019 Nov 26;9(1):317.
Liu, Z., et al. Tight junctions, leaky intestines, and pediatric diseases. Acta Paediatricia. 94 (2005): 386-393.
Madra, M., et al. Gastrointestinal Issues and Autism Spectrum Disorder. Psychiatr Clin North Am. 2021 Mar; 44(1): 69–81.
Manichanh, C., et al. The gut microbiota in IBD. Nat Rev Gastroenterol Hepatol. 2012;9(10):599-608.
Mattila, K., et al. Burden of illness and use of health care services before and after celiac disease diagnosis in children. J Pediatr Gastroenterol Nutr. 2013;57(1):53-6
Mine, Y., et al. Surfactants Enhance the Tight-Junction Permeability of Food Allergens in Human Intestinal Epithelial Caco-2 Cells. International Archives of Allergy and Immunology. 2003 Feb;130(2):135-42.
Mitre, E., et al. Association Between Use of Acid-Suppressive Medications and Antibiotics During Infancy and Allergic Diseases in Early Childhood. JAMA Pediatr. 2018 Jun 4;172(6):e180315.
Mohan, R., et al. Effects of Bifidobacterium lactis Bb12 Supplementation on Intestinal Microbiota of Preterm Infants: A Double-Blind, Placebo-Controlled, Randomized Study. Journal of Clinical Microbiology. 2006 Nov;44(11):4025-31.
Möller, C., et al. Intestinal permeability as assessed with polyethyleneglycols in birch pollen allergic children undergoing oral immunotherapy. Allergy. 1986 May;41(4):280-5.
Montalto, M., et al. Fecal Calprotectin Concentrations in Patients with Small Intestinal Bacterial Overgrowth. Digestive Diseases. 2008;26(2):183-6.
Morris, C.R., et al. Syndrome of allergy, apraxia, and malabsorption: characterization of a neurodevelopmental phenotype that responds to omega 3 and vitamin E supplementation. Alternative Therapies in Health and Medicine. Jul-Aug 2009;15(4):34-43.
Moser, L.A. Astrovirus Increases Epithelial Barrier Permeability Independently of Viral Replication. Journal of Virology. 2007 Nov;81(21):11937-45.
Nankova, B.B., et al. Enteric bacterial metabolites propionic and butyric acid modulate gene expression, including CREB-dependent catecholaminergic neurotransmission, in PC12 cells–possible relevance to autism spectrum disorders. PLoS One. 2014;9(8):e103740.
Nankova, B.B. Nicotinic Induction of Preproenkephalin and Tyrosine Hydroxylase Gene Expression in Butyrate-Differentiated Rat PC12 Cells: A Model for Adaptation to Gut-Derived Environmental Signals. Pediatric Research. 2003 Jan;53(1):113-8.
Nemechek, P., et al. Autism Spectrum Disorder Symptoms Improve with Combination Therapy Directed at Improving Gut Microbiota and Reducing Inflammation. Applied Psychiatry. 2020 Jul; (1)1.
Niederhofer, H., et al. A preliminary investigation of ADHD symptoms in persons with celiac disease. J Atten Disorder. 2006 Nov;10(2):200-4.
Nirmalkar, K., et al. Shotgun Metagenomics Study Suggests Alteration in Sulfur Metabolism and Oxidative Stress in Children with Autism and Improvement after Microbiota Transfer Therapy. Int J Mol Sci. 2022 Nov 3;23(21):13481.
Nikolova, V.L., et al. Acceptability, Tolerability, and Estimates of Putative Treatment Effects of Probiotics as Adjunctive Treatment in Patients With Depression. JAMA Psychiatry. 2023 Aug 1;80(8):842-847.
Nirmalkar, K., et al. Shotgun Metagenomics Study Suggests Alteration in Sulfur Metabolism and Oxidative Stress in Children with Autism and Improvement after Microbiota Transfer Therapy. Int J Mol Sci. 2022 Nov 3;23(21):13481.
O’Hara, A.M., et al. The gut flora as a forgotten organ. European Molecular Biology Organization Report 7, no 7 (July 2006): 688-693.
Oliva-Hemker, M., et al. Fecal Microbiota Transplantation: Information for the Pediatrician. Pediatrics. 2023 Dec 1;152(6):e2023062922.
Ozkul, C., et al. A single early-in-life antibiotic course increases susceptibility to DSS-induced colitis. Genome Med. 2020;12(1):65.
Parkin, K.,, et al. Risk Factors for Gut Dysbiosis in Early Life. Microorganisms. 2021 Sep 30;9(10):2066.
Pearson, A.D., et al. Intestinal permeability in children with Crohn's disease and coeliac disease. Br Med J (Clin Res Ed). 1982 Jul 3;285(6334):20-1.
Rautava, S., et al. The Development of Gut Immune Responses and Gut Microbiota: Effects of Probiotics in Prevention and Treatment of Allergic Disease. Current Issues in Intestinal Microbiology. 2002 Mar;3(1):15-22.
Rediers, H., et al. Unraveling the Secret Lives of Bacteria: Use of In Vivo Expression Technology and Differential Fluorescence Induction Promoter Traps as Tools for Exploring Niche-Specific Gene Expression. Microbiology and Molecular Biology Reviews. 2005 Jun;69(2):217-61.
Relman, D.A. The human microbiome: ecosystem resilience and health. Nutr Rev. 2012 Aug;70 Suppl 1(Suppl 1):S2-9.
Ristori, M.V., et al. Autism, Gastrointestinal Symptoms and Modulation of Gut Microbiota by Nutritional Interventions. Nutrients. 2019;11:2812.
Rook, G.A., et al. Microbiota, immunoregulatory old friends and psychiatric disorders. Adv Exp Med Biol. 2014;817:319-56.
Rowland, I.R., et al. Effects of diet on mercury metabolism and excretion in mice given methylmercury: role of gut flora. Archives of Environmental Health. Nov-Dec 1984;39(6):401-8.
Sanchez, A., et al. Role of sugars in human neutrophilic phagocytosis. Am J Clin Nutr. 1973 Nov;26(11):1180-4.
Savino, F., et al. Lactobacillus reuteri (American Type Culture Collection Strain 55730) versus simethicone in the treatment of infantile colic: a prospective randomized study. Pediatrics. 2007 Jan;119(1):e124-30.
Scirocco, A., et al. Exposure of Toll-like receptors 4 to bacterial lipopolysaccharide (LPS) impairs human colonic smooth muscle cell function. J Cell Physiol. 2010 May;223(2):442-50.
Sela, D.A., et al. The marriage of nutrigenomics with the microbiome: the case of infant associated bifidobacteria and milk. Am J Clin Nutr. 2014;99(3):697S-703S.
Severance, E.G., et al. IgG dynamics of dietary antigens point to cerebrospinal fluid barrier or flow dysfunction in first-episode schizophrenia. Brain Behav Immun. 2015 Feb;44:148-58.
Shekhawat, P.S., et al. Spontaneous development of intestinal and colonic atrophy and inflammation in the carnitine-deficient jvs (OCTN2(-/-)) mice. Mol Genet Metab. 2007 Dec;92(4):315-24.
Sifroni, K.G., et al. Mitochondrial respiratory chain in the colonic mucosal of patients with ulcerative colitis. Mol Cell Biochem. 2010 Sep;342(1-2):111-5.
Simpson, C.A., et al. The gut microbiota in anxiety and depression - A systematic review. Clin Psychol Rev. 2021 Feb:83:101943.
Stewart, C.J., et al. Temporal development of the gut microbiome in early childhood from the TEDDY study. Nature. 2018 Oct;562(7728):583-588.
Strauch, U.G., et al. Influence of intestinal bacteria on induction of regulatory T cells: lessons from a transfer model of colitis. Gut 54 (2005):1546-1552.
Strandwitz, P. Neurotransmitter Modulation by the Gut Microbiota. Brain Res. 2018 Aug 15;1693(Pt B):128-133.
Tobacman, J.K. Review of Harmful Gastrointestinal Effects of Carrageenan in Animal Experiments. Environmental Health Perspectives. 2001 Oct;109(10):983-94.
Uhde, M., et al. Intestinal cell damage and systemic immune activation in individuals reporting sensitivity to wheat in the absence of coeliac disease. Gut. 2016 Dec;65(12):1930-1937.
Vael, C., et al. Early intestinal Bacteroides fragilis colonization and development of asthma. BMC Pulmonary Medicine. 2008 Sep 26;8:19.
van Nood, E., et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013 Jan 31;368(5):407-15.
Videhult, F.K., et al. Impact of probiotics during weaning on the metabolic and inflammatory profile: follow-up at school age. Int J Food Sci Nutr. 2015;66(6):686-91.
Voigt, R.M., et al. The intestinal microbiota: determinants of resiliency? Lancet Healthy Longev. 2021 Jan;2(1):e2-e3.
Vojdani, A., et al. A Gut Feeling for Immune Dysregulation & Neuroinflammation in Autism. The Autism File. 2009(31).
Wang, J., et al. Global Prevalence of Autism Spectrum Disorder and Its Gastrointestinal Symptoms: A Systematic Review and Meta-Analysis. Front. Psychiatry. 2022;13:963102.
Warner, B.B. The contribution of the gut microbiome to neurodevelopment and neuropsychiatric disorders. Pediatr Res. 2019 Jan;85(2):216-224.
Wasilewska, J., et al. Gastrointestinal symptoms and autism spectrum disorder: links and risks – a possible new overlap syndrome. Pediatric Health Med Ther. 2015; 6: 153–166.
West, C.E., et al. The gut microbiota and inflammatory noncommunicable diseases: associations and potentials for gut microbiota therapies. J Allergy Clin Immunol. 2015;135(1):3-13; quiz 4.
Wexler, H. Bacteroides: the Good, the Bad, and the Nitty-Gritty. Clinical Microbiology Reviews 20, no. 4 (October 2007): 593-621.
White, E., et al. The Effect of Nutritional Therapy for Yeast Infection (Candidiasis) in Cases of Chronic Fatigue Syndrome. Journal of Orthomolecular Medicine. 2005;20(3).
Williams, B.L., et al. Impaired Carbohydrate Digestion and Transport and Mucosal Dysbiosis in the Intestines of Children with Autism and Gastrointestinal Disturbances. PLoS ONE. 2011;6:e24585.
Williams, R.E.O., et al. The influence of intestinal bacteria on the absorption and metabolism of foreign compounds. Journal of Clinical Pathology.1971; 5: 125–129.
Wilmanski, T., et al. Gut microbiome pattern reflects healthy ageing and predicts survival in humans. Nat Metab. 2021 Feb;3(2):274-286.
Yang, B., et al. Effects of regulating intestinal micobiota on anxiety symptoms: A systematic review. General Psychiatry. 2019; 32: e100056.
Zheng, P., et al. Gut microbiome in type 1 diabetes: A comprehensive review. Diabetes Metab Res Rev. 2018 Oct;34(7):e3043.
Zhou, H., et al. Evaluating the Causal Role of Gut Microbiota in Type 1 Diabetes and Its Possible Pathogenic Mechanisms. Front Endocrinol (Lausanne). 2020 Mar 24:11:125.
Zhu, B., et al. Human gut microbiome: the second genome of human body. Protein Cell. 2010 Aug;1(8):718-25.
Resources
Books
Galland, Leo. The Effect of Intestinal Microbes on Systemic Immunity. Excerpted from Power Healing. Random House, 1998.
Lambert, Beth. A Compromised Generation: The Epidemic of Chronic Illness in America’s Children. Sentient Publications, 2010.
Sachs, Jessica Snyder. Good Germs, Bad Germs: Health and Survival in a Bacterial World. Hill and Wang, 2007.