Visual processing disorder (VPD) is a neurological condition in which the brain has trouble interpreting and making sense of visual information received from the eyes, despite clear eyesight. These challenges often go unrecognized in children and adults, yet they play a critical role in how we learn, interact, and experience the world.
The Difference Between Acuity and Vision
While many assume that “vision” means simply seeing clearly, it does not. Acuity is how well we see at a distance (such as 20/20) and refers to nearsightedness or farsightedness. For example, acuity is the ability to see letters on a chart clearly.
Vision is how the brain processes the information coming in through the eyes. It is the complex coordination between the two eyes and the brain to create meaning from what is seen, allowing a person to understand his or her surroundings, interact socially, and perform daily tasks. The process entails being able to track, focus, coordinate, and integrate visual information with other sensory and motor tasks.
What Is Visual Processing Disorder?
At its core, a visual processing disorder is not just about poor eyesight or the need for glasses. It refers to difficulties in the brain’s ability to make sense of visual information. Visual-processing challenges are about function: how you take in, interpret, and act upon the world around you. These difficulties commonly go overlooked, even in conventional eye exams, because standard tests usually focus on acuity rather than issues such as:
- How well the eyes track together
- How efficiently visual information is processed
- If the neural mechanisms responsible for turning sight into understanding are functioning properly
This often leads to problems being undetected, misdiagnosed, or mistakenly categorized purely as behavioral or learning issues. Many children and adults struggle not with “seeing” but with “making sense” of what they see. When a child has visual processing disorder, his or her brain may fail to successfully integrate information from the eyes, resulting in difficulties with everyday tasks. Such children may pass standard eye exams and have “20/20 vision” but still struggle with tasks requiring the eyes and brain to work together. Common signs include:
- Difficulty tracking lines while reading and writing
- Losing place when reading
- Skipping words or lines
- Confusing letters or numbers
- Words moving, blurring, or going in and out of focus
- Problems copying from the board to paper
- Clumsiness or poor coordination in sports or play
- Resistance to reading
- Complaints of eye strain
- Struggling to read
- Lacking confidence
- Feeling frustration
- Problems with social interactions
- Difficulty with self-regulation
- Feeling fatigued, especially during work or school
- Chronic headaches
- Lack of depth perception
- A feeling of being lazy or stupid
- Difficulty focusing for extended periods
- A negative association with sustained desk work
Visual processing involves a range of skills, including:
- Fixation: The ability to look at and maintain focus on an object
- Tracking (pursuit and saccadic eye movements): Following a moving object or jumping from word group to word group while reading
- Fusion (eye teaming): Coordinating both eyes to see a single image
- Focusing (accommodation): Shifting focus quickly and accurately between near and far objects
Weakness in any of these areas can disrupt learning, physical coordination and self-esteem. It’s important to remember that these are not simply issues of “bad behavior” or lack of effort, but rather neurobiological challenges requiring targeted intervention.
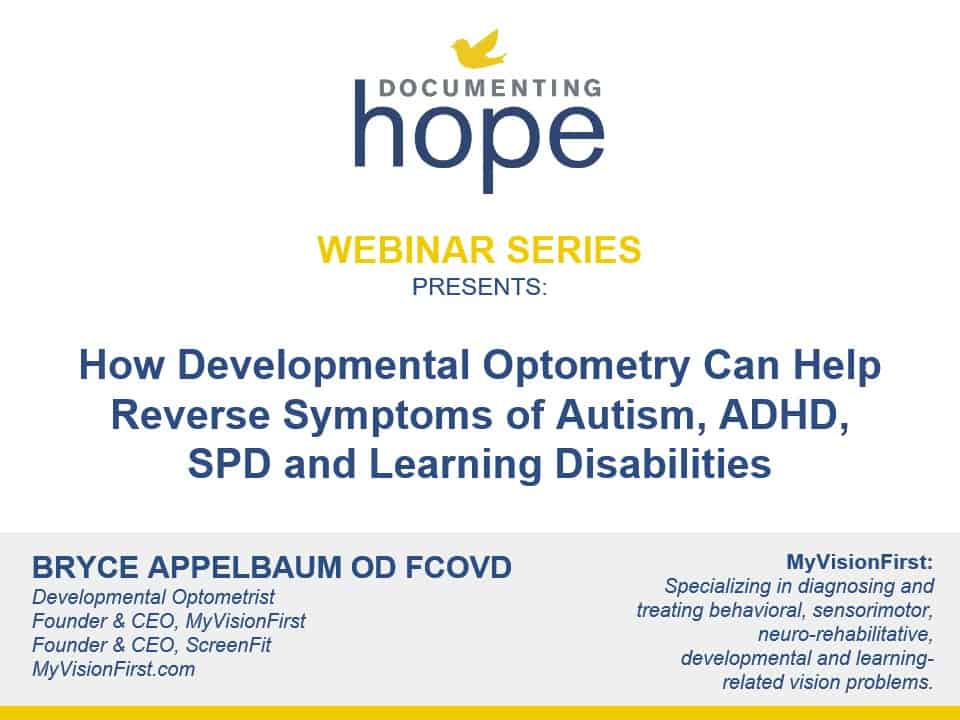
What Types of Conditions Often Have a Visual Processing Disorder Component?
Visual-processing challenges can be standalone issues or exist alongside broader diagnoses, affecting children and adults with a range of developmental, neurological, and learning challenges. In particular, autism, ADD/ADHD, learning disabilities and dyslexia are often incomplete diagnoses until looking at or addressing vision first because their symptoms and behaviors can overlap significantly with those arising from undetected visual-processing deficits. We strongly encourage looking for underlying vision problems before accepting these diagnoses at face value. Following are conditions that often have a visual processing disorder component:
Autism Spectrum Disorder (ASD)
Children with autism frequently experience challenges with visual attention, tracking, double vision and the integration of visual information. Avoiding eye contact, sideways glancing, “visual stimming” (hand flapping, flicking things near the face, lining up toys and other objects), and difficulty with visual-spatial organization are all common symptoms of autism.
Children with autism often have difficulties with visual fixation (keeping the eyes on a target) and integrating central and peripheral vision. These are extra hurdles for kids trying to communicate using motor-based methods such as Spelling to Communicate (S2C) or typing. Spellers Method practitioners collaborate with developmental optometrists to personalize communication tools—such as choosing the right color and type of letterboard—to better suit a child’s specific visual needs. This approach makes it easier for them to reliably point to letters and express themselves.
Supporting vision is fundamental to improving intentional motor skills and communication outcomes for children with autism. The Spellers Method addresses vision, sensory integration, reflex issues, and motor planning together so that those with autism have a much greater chance of successful, reliable communication—whether through speech or alternative methods such as Spelling to Communicate.
Attention Deficit Disorders (ADD and ADHD)
While ADHD and ADD are typically thought of as a behavioral or attentional issue, underlying visual-processing weaknesses can exacerbate symptoms. A child may struggle to maintain visual focus, look up from their paper, or follow directions on a board simply because their visual systems aren’t working efficiently.
Sensory Processing Disorder (SPD)
SPD affects the ability to interpret and respond to sensory input, which includes visual information. Children may compensate for weak visual processing by over-relying on other senses such as touch (tactile) and muscle/joint feedback (proprioception), sometimes leading to “hands everywhere” behaviors or sensory defensiveness.
Learning Disabilities (LD), Including Dyslexia
Dyslexia and other learning disabilities can involve problems with the speed and efficiency with which the brain decodes visual symbols (letters, numbers, patterns). Difficulties with eye movement, tracking across a page, or visual memory can impact the ability to read and spell efficiently.
PANS/PANDAS and Lyme Disease
Many children with visual processing disorder may unknowingly have PANS/PANDAS and/or Lyme disease. The reverse is also true: Children with PANS/PANDAS and/or Lyme disease may also have visual processing disorder. Read the success story here of Whitman, whose vertigo forced him into a wheelchair until William Padula OD SFNAP FAAO FNORA diagnosed him with Visual Midline Shift Syndrome, which was causing accommodative spasms and his vertigo. Dr. Padula recommended treatment with asymmetrical prisms and noted a ring around the optic nerve that is a biomarker of Lyme disease. You can purchase our 2024 conference videos here, in which Dr. Padula presented Whitman’s case study.
Mold, Mycotoxin and Biotoxin Illnesses
In our experience, if a child has plateaued in their healing, there is often an undiagnosed mold, mycotoxin and biotixin illness for the child either in home or at school. See Ritchie Shoemaker MD’s Visual Contrast Sensitivity (VCS) test, which can be performed inexpensivlely and online, to determine if mold is affecting your child’s visual processing.
Brain Injuries and Neurological Conditions
Conditions such as brain injury, concussion, or illnesses such as multiple sclerosis can disrupt normal visual-processing pathways. In some cases, people with these conditions develop difficulties with double vision, field loss, or spatial judgment after injury or illness.
Strabismus and Amblyopia
Strabismus is when one eye turns in, out, up, or down, and amblyopia refers to a “lazy eye” where the brain ignores input from one eye. These conditions disrupt the ability to achieve binocular (two-eyed) vision, making depth perception and spatial awareness difficult. Sometimes these problems are only visible under certain lighting or after fatigue, complicating diagnosis. Interestingly, surgery to fix a lazy eye often has only a cosmetic effect and does not change the visual-processing challenge.
Convergence Insufficiency
This condition refers to the eyes’ inability to coordinate together when focusing on near tasks such as reading. Children may experience double vision or fatigue, which can impact reading and learning. Unfortunately, standard vision tests may not pick up on this.
Dyspraxia and Apraxia
Visual-motor dysfunction involves difficulties in coordinating eye movement with motor actions, affecting everything from handwriting to sports participation. Vision is intertwined with motor planning because of the way the body and brain are wired together during a baby’s development. Therefore, a child with dyspraxia or apraxia is likely to also have visual processing disorder.
Non-Verbal Communication and Emotional Regulation
Visual processing is critical for reading non-verbal cues, facial expressions, and social interactions. When visual-processing challenges go unresolved, children may struggle socially, which can be mistaken for behavioral problems.
“Hidden” Vision Problems
Even without a formal diagnosis, many students and adults struggle to thrive at school, work, or in sports due to undetected visual-processing challenges.
How Does a Baby’s Development Affect Visual-Processing Challenges?
Visual processing disorder is common in children with developmental delays, particularly those who didn’t crawl properly (or at all), missed certain physical milestones, or developed maladaptive habits due to prematurity, birth trauma, or other medical issues. Motor milestones and reflex integration directly affect visual processing later in life. Vision does not develop in isolation; rather, it is deeply connected to foundational motor skills. Early clues of a visual processing disorder might include:
Babies who don’t track moving objects or make consistent eye contact by 6–8 months
- Ongoing crossed or drifting eyes beyond early infancy
- Delays in reaching, crawling, or exploring the environment visually
- Continued mouthing or excessive touching of toys (compensating for poor visual curiosity or understanding)
Why Crawling on Hands and Knees Matters
Crawling on hands and knees, which is not the same as army crawling, is an essential milestone in brain development and visual processing because it wires the brain and body together for optimal vision. We recommend that you disregard the Center for Disease Control’s (CDC) guidance of saying that it’s okay if your baby skips crawling altogether; it’s not okay. (Please also read our article, The CDC Has Worsened Developmental Delays).
Crawling is not just about physical development; it is fundamentally linked to integrating the two hemispheres of the brain, establishing handedness (laterality), bilateral integration, reciprocal movement, improving core strength, and coordinating the eyes and hands. Crawling supports the development of visual-motor integration and spatial awareness. When a baby crawls, the eyes follow the hands, facilitating the development of the visual system’s connection with the motor system.
Missing or performing this milestone incorrectly (such as crawling asymmetrically, butt scooting, army crawling instead of on hands and knees, or crawling with a leg out to the side) can result in persistent visual-processing problems. Children who skip or shorten this milestone often later exhibit challenges with vision, coordination, and learning. In addition, they are much more likely to be diagnosed with a neurodevelopmental disorder such as autism, ADHD, SPD or a learning disability. Therapists sometimes reintroduce crawling exercises to “reinstate” this critical developmental stage and stimulate hemispheric and sensory integration, even in older children and adults. Learn more here from Sarge Goodchild about How a Child’s Brain Develops.
Reflex Integration
Underlying reflexes, such as the asymmetrical tonic neck reflex (ATNR) and symmetrical tonic neck reflex (STNR), play a key role in visual and motor development. If these reflexes are not integrated properly—possibly due to missed milestones such as crawling—a cascade of issues, including retained primitive reflexes, can arise. These, in turn, affect how the eyes work together and how the brain processes visual information.
Environmental Factors
Early development is also impacted by environment and lifestyle. Exposure to screens at a young age, lack of tummy time, back sleeping, being kept in confined containers such as baby carriers, and missing critical periods for visual development can exacerbate problems.
The transition from a visually rich outdoor environment to intense near work and digital screens is contributing to more visual-processing challenges in children than ever before. Societal shifts toward early academic pressure and technology amplify these effects. Children are asked to read before their visual system is ready, and an abundance of screen time increases near-vision stress while depriving the brain of necessary outdoor and active experiences. The average eight year old spends six hours daily on screens—a stunning amount of time. This can result in dramatic rises in visual developmental delays, nearsightedness (myopia), and related learning difficulties.
Follow-On Effects of Visual Processing Disorder
Because vision is the dominant sense of the body and uses about 80% of the brain’s processing power, the ripple effect on the rest of the body is significant. If the visual system is stressed, strained or not working optimally, children with visual processing disorder often also have:
- Allergies
- Food sensitivities and intolerances
- Speech and language difficulties
- Asthma
- Auditory processing disorder
- Gastrointestinal disorders
- Motion sickness
- Colic
- Eczema
When visual difficulties are addressed and remediated with appropriate therapy and/or supports, parents often note that their children’s other health challenges, such as those listed above, may abate or improve. This is due to the undue stress that visual processing disorder places on the brain’s and body’s resources. If these resources are no longer being deployed to address vision challenges, then they can be used elsewhere in the body to help the body address its backlog of healing.
What Can Be Done About Visual Processing Disorder?
The good news is that visual-processing challenges are both identifiable and highly treatable—and addressing them can unlock profound improvements in a child’s learning, regulation, and well-being. With the right evaluation, interventions, and ongoing collaboration among specialists, parents, and educators, children can thrive and overcome many of their challenges associated with this disorder.
Assessment
Start with a Detailed History
The first step is always a thorough history. Understanding the child’s developmental trajectory—including delays or skipped milestones such as crawling or walking—and looking for soft signs such as colic, eczema, or missing milestones is important. This history should go beyond what happened yesterday or last year and look into prenatal, family, and even generational factors.
Seek the Right Professional for a Comprehensive Vision Evaluation
Conventional optometrists typically won’t catch a visual processing disorder. A standard “20/20” vision screening at school or the pediatrician’s office is NOT enough. Most of these kinds of screenings miss subtle but important vision problems linked to learning and development.
Instead, you’ll want to find someone who is board-certified as a behavioral optometrist, a developmental optometrist or a neuro-optometrist. These specialized optometrists will usually have “FCOVD” listed after their names. This means that can perform specialized tests that involve evaluating and retraining how the eyes move, focus, and coordinate, as well as how the brain organizes and processes visual information. Unlike the reactive medical model that waits for disease or structural breakdown, developmental optometrists take a proactive approach focused on enhancing function. You can find one in your area by visiting the Optometric Vision Development and Rehabilitation Association at https://www.covd.org/
Although most of these practitioners work with children and adults with neurodevelopmental disorders, traumatic brain injury and neurological symptoms, some of them work only with athletes who want be at the top of their game by optimizing hand-eye coordination. Be sure to check out a prospective doctor’s website or call their office to determine if he or she could be a good fit for your child.
We recommend:
- All infants should receive an eye exam in their first year (the American Optometric Association’s InfantSEE program offers free checks for infants under one).
- Preschoolers (by age three), then before starting school, and every year thereafter should have an exam by an eye doctor—preferably one trained in developmental or behavioral optometry.
- Children with learning or developmental issues should receive a comprehensive vision exam, including “near point” (within arm’s reach) assessment and specific tests for tracking, focusing, and visual processing.
Tests for convergence, binocular coordination, tracking, and sometimes reflex integration that are performed by developmental optometrist are critical. Observing how a child responds to visual tasks, their posture when reading, their perception of depth (such as when walking up or down stairs), and even their behavior in environments with different lighting conditions provides important clues. Sometimes children who see double or struggle visually do not mention it because they don’t know that’s not everybody’s experience.
Remediation
Vision Therapy
Vision therapy is designed to rehabilitate the visual system in concert with the brain. Vision therapy can transform lives, helping children and adults integrate visual input, improve depth perception, and support learning and motor skills. It is an individualized, brain-based treatment plan designed to remediate visual-processing deficits. Typically overseen by a developmental optometrist and highly trained therapists, vision therapy includes:
- Exercises to improve eye tracking, focusing, coordination and depth perception
- Strengthening of eye coordination (convergence and divergence)
- Building visual memory and integration
- Enhancing central and peripheral awareness simultaneously
- Supporting self-regulation and organized, intentional movement
- Integration of visual skills with motor, balance, and sensory activities
- Use of lenses, prisms, or tints as therapeutic tools—not just to help “see better,” but to reorganize how the visual system interacts with the body and environment
Vision therapy can be adapted for children (and adults) on the autism spectrum, as well as those with ADHD, dyslexia, SPD, learning disabilities and even brain injury. Programs are tailored to each individual’s needs, taking into account strengths, deficits, daily living goals, and neurological profile. Activities are engaging and often play-based, incorporating tactile, proprioceptive, and balance-challenging elements. Children and adults who have vision therapy can overcome clumsiness, improve their handwriting, dramatically reduce frustration, and often improve academically and socially after treatment.
Visualization and Cognitive Strategies
An important—but often overlooked—part of vision is visualization, or the ability to create “mental movies” of what one reads, plans, or imagines. Lynn Hellerstein OD FCOVD describes using visualization in therapy to support reading comprehension, spelling, math facts, sports performance, creative writing, and managing anxiety.
Visualization techniques can make abstract concepts tangible and memorable—think drawing colorful flashcards, using creative imagery to learn words, or mentally rehearsing athletic moves. Dr. Hellerstein notes that effective learners, including athletes and strong readers, make frequent use of visualization.
Collaboration with Other Professionals
Many children and adults with neurodevelopmental challenges benefit from a combination of interventions—occupational therapy for sensory integration, nutrition, neurological healing, and developmental optometry. Collaboration among practitioners—along with parental intuition and documentation—helps optimize outcomes and track progress. For children with tactile or proprioceptive sensitivities, therapists may recommend strategies to help them tolerate glasses, frames, or new routines.
Occupational Therapy
Occupational therapists are often key players as they address sensory integration, reflexes, and motor planning issues that underlie visual-processing challenges. (Please note, however, that most occupational therapists are not trained in reflex integration; you’ll need to do some detective work to find out if they’re trained in this.) Combining vision therapy with movement, using swings or scooter boards, can deliver powerful results for children with speech and visual-motor challenges.
Reflex Integration Therapy
Reflex-integration therapies such as Masgutova Neurosensory Reflex Integration (MNRI), rhythmic movement and crawling exercises are designed to address retained reflexes, improve hemispheric integration, and lay a stronger foundation for vision and learning.
Lifestyle and Environmental Changes
Improving the environment with adequate lighting, reducing screen time, and encouraging outdoor play as well as addressing nutrition (such as whole foods, including healthy fats for myelinating nerves), sleep quality, and removal of sensory stressors can support visual development and remediation. Managing inflammation through diet and lifestyle is also key, since inflammation can disrupt neurological and visual function.
Practical Accommodations and Home Strategies
Simple changes at home can make a big difference for a child with visual processing disorder:
- Using an angled posture board or slanted desk for reading/writing can help tracking and reduce eye fatigue.
- Allowing breaks and building endurance for sustained visual tasks.
Personalized Plans
Remember that there is no one-size-fits-all solution. Everyone’s needs are different—and what works for one child may not work for another.
Emotional Support and Advocacy
It is important not to pathologize behavior as simply “bad” but instead to recognize it as communication and a call for help. Children with visual-processing challenges should have their needs seen, heard, and acknowledged—with a focus on their strengths, potential for transformation, and right to a life unhindered by misunderstood neurobiological challenges.
Conclusion
Visual processing disorder affects many children, often silently undermining learning, social engagement, and emotional regulation. Early motor development—especially crawling and reflex integration—plays a decisive role in setting the stage for visual processing throughout life.
With proper history-taking, targeted professional assessments, and personalized interventions, it’s possible not just to manage but to transform the trajectory for children and adults with visual-processing challenges. The right support offers hope, healing, and—most importantly—a life of greater possibility and connection. Addressing visual-processing disorder not only helps reverse symptoms—it unlocks human potential in learning, social life, and self-confidence.
About Maria Rickert Hong CHHC
Maria Rickert Hong is a Co-Founder of, and the Education and Media Director for, Documenting Hope.
She is a former sell-side Wall Street equity research analyst who covered the oil services sector at Salomon Smith Barney and Lehman Brothers under Institutional Investor #1 ranked analysts.
Later, she covered the gaming, lodging & leisure sector at Jefferies & Co. and Calyon Securities. She quit working on Wall Street when her first son was born.
Prior to working on Wall Street, she was a marketing specialist for Halliburton in New Orleans, where she also received her MBA in Finance & Strategy from Tulane University.
She is the author of the bestselling book Almost Autism: Recovering Children from Sensory Processing Disorder and the co-author of Brain Under Attack: A Resource for Parents and Caregivers of Children with PANS, PANDAS, and Autoimmune Encephalitis. She is a co-author of Reversal of Autism Symptoms among Dizygotic Twins through a Personalized Lifestyle and Environmental Modification Approach: A Case Report and Review of the Literature, J. Pers. Med. 2024, 14(6), 641.
Maria is also a Certified Holistic Health Counselor. Her work can be found on DocumentingHope.com, Healing.DocumentingHope.com, Conference.DocumentingHope.com and MariaRickertHong.com
Still Looking for Answers?
Visit the Documenting Hope Practitioner Directory to find a practitioner near you.
Join us inside our online membership community for parents, Healing Together, where you’ll find even more healing resources, expert guidance, and a community to support you every step of your child’s healing journey.
Sources & References
Bakroon, A., et al. Visual function in autism spectrum disorders: a critical review. Clin Exp Optom. 2016 Jul;99(4):297-308.
Bellato, A., et al. Association between ADHD and vision problems. A systematic review and meta-analysis. Mol Psychiatry. 2023 Jan;28(1):410-422.
Bertone, A., et al. Enhanced and diminished visuo-spatial information processing in autism depends on stimulus complexity. Brain. 2005 Oct;128(Pt 10):2430-41.
Chang, M.Y., et al. Prevalence of Ophthalmologic Diagnoses in Children With Autism Spectrum Disorder Using the Optum Dataset: APopulation-Based Study. Am J Ophthalmol. 2021 Jan:221:147-153.
Davis, R.A.O., et al. Subjective perceptual distortions and visual dysfunction in children with autism. J Autism Dev Disord. 2006 Feb;36(2):199-210.
DeCarlo, D.K., et al. Prevalence of attention-deficit/hyperactivity disorder among children with vision impairment. J AAPOS. 2014 Feb;18(1):10-4.
De Jonge, M.V., et al. Visual information processing in high-functioning individuals with autism spectrum disorders and their parents. Neuropsychology. 2007 Jan;21(1):65-73.
Egset, K., et al. Magno App: Exploring Visual Processing in Adults with High and Low Reading Competence. Scandinavian Journal of Educational Research. 07 Jan 2020.
Franklin, A., et al. Reduced chromatic discrimination in children with autism spectrum disorders. Dev Sci. 2010 Jan 1;13(1):188-200.
Grigg. T.M., et al. Primitive Reflex Integration and Reading Achievement in the Classroom. Journal of Neurology and Experimental Neuroscience. 2023; 9(1), 18-26.
Ho, J.D., et al. Associations between attention-deficit/hyperactivity disorder and ocular abnormalities in children: a population-based study. Ophthalmic Epidemiol. 2020 Jun;27(3):194-199.
Kaplan, M., et al. Strabismus in Autism Spectrum Disorder. Focus on Autism and Other Developmental Disabilities. 1999.
Koh, H.C., et al. Spatial contrast sensitivity in adolescents with autism spectrum disorders. J Autism Dev Disord. 2010 Aug;40(8):978-87.
Johnson, B.P., et al. Ocular motor disturbances in autism spectrum disorders: systematic review and comprehensive meta-analysis. Neurosci Biobehav Rev. 2016 Oct:69:260-79.
Khanna, R.K., et al. Ophthalmological findings in children with autism spectrum disorder. Graefes Arch Clin Exp Ophthalmol. 2020 Apr;258(4):909-916.
Little, J.A. Vision in children with autism spectrum disorder: a critical review. Clin Exp Optom. 2018 Jul;101(4):504-513.
Maron, D.N., et al. Oculomotor deficits in attention deficit hyperactivity disorder (ADHD): a systematic review and comprehensive meta-analysis. J Autism Dev Disord. 2006 Feb;36(2):199-210.
Milne, E., et al. Vision in children and adolescents with autistic spectrum disorder: evidence for reduced convergence. J Autism Dev Disord. 2009 Jul;39(7):965-75.
Mouridsen, S.E., et al. Eye Disorders among Adult People Diagnosed with Infantile Autism in Childhood: A Longitudinal Case Control Study. Ophthalmic Epidemiol. 2017 Oct;24(5):332-335.
Padula, W.V., et al. Modifying postural adaptation following a CVA through prismatic shift of visuo-spatial egocenter. Brain Inj. 2009 Jun;23(6):566-76.
Padula, W.V., et al. Risk of fall (RoF) intervention by affecting visual egocenter through gait analysis and yoked prisms. NeuroRehabilitation. 2015;37(2):305-14.
Padula, W.V., et al. The consequence of spatial visual processing dysfunction caused by traumatic brain injury (TBI). Brain Inj.. 2017;31(5):589-600.
Padula, W.V., et al. Visual evoked potentials (VEP) evaluating treatment for post-trauma vision syndrome (PTVS) in patients with traumatic brain injuries (TBI). Brain Inj. 1994 Feb-Mar;8(2):125-33.
Perna, J., et al. Association between Autism Spectrum Disorder (ASD) and vision problems. A systematic review and meta-analysis. Mol Psychiatry. 2023 Dec;28(12):5011-5023.
Reimelt, C., et al. The underestimated role of refractive error (hyperopia, myopia, and astigmatism) and strabismus in children with ADHD. J Atten Disord. 2021 Jan;25(2):235-244.
Robertson, C.E., et al. Tunnel vision: sharper gradient of spatial attention in autism. J Neurosci. 2013 Apr 17;33(16):6776-81.
Sarno, S., et al. Electrophysiological correlates of visual impairments after traumatic brain injury. Vision Res. 2000;40(21):3029-38.
Simmons, D.R., et al. Vision in autism spectrum disorders. Vision Res. 2009 Nov;49(22):2705-39.
Stephens-Sarlós, E., et al. The efficacy of the sensorimotor training program on sensorimotor development, auditory and visual skills of schoolchildren aged 5–8 years. Child & Youth Care Forum. 2024 Aug;54(2):323-352.
Song, Y., et al. Can they see it? The functional field of view is narrower in individuals with autism spectrum disorder. PLoS One. 2015 Jul 23;10(7):e0133237.
Su, C.C., et al. Incidence and risk of attention-deficit hyperactivity disorder in children with amblyopia: a nationwide cohort study. Clin Exp Ophthalmol. 2019 Mar;47(2):259-264.
Van der Hallen, R., et al. Global Motion Perception in Autism Spectrum Disorder: A Meta-Analysis. J Autism Dev Disord. 2019 Dec;49(12):4901-4918.
Wang, J., et al. Refractive Status and Amblyopia Risk Factors in Chinese Children with Autism Spectrum Disorder. J Autism Dev Disord. 2018 May;48(5):1530-1536.
Whatham, A., et al. Vitamin and mineral deficiencies in the developed world and their effect on the eye and vision. Ophthalmic Physiol Opt. 2008 Jan;28(1):1-12.
Resources
Articles
CBS Chicago: Vision Problems In Kids Can Be Misdiagnosed For ADHD
Move, Play, Thrive: Vision Doctor on Rhythmic Movements + Research about Visual Processing Issues.
Books
Hellerstein, Lynn. 50 Tips to Improve Your Sports Performance. HiClear Publishing LLC, 2013.
Hellerstein, Lynn. Expand Your Vision Beyond Sight.HiClear Publishing LLC, 2012.
Hellerstein, Lynn. Organize It. HiClear Publishing LLC, 2010.
Hellerstein, Lynn. See It, Say It, Do It. HiClear Publishing LLC, 2012.
Lemer, Patricia S. Envisioning a Bright Future: Interventions That Work for Children and Adults with Autism Spectrum Disorders. Optometric Extension Program Foundation, 2008.
Videos
Catching a Ball for the First Time at 39: Justin’s Story
Vision Therapy Transformed Our Son’s Life: Atlas’ Story
Websites
Neuro-Optometric Rehabilitation Association
Optometric Vision Development Rehabilitation Association